A widely available nasal spray may help prevent COVID-19 infections, according to recent clinical trial results. The over-the-counter antihistamine azelastine, long used to treat seasonal allergies, appears to work as an antiviral against multiple respiratory viruses, including influenza, RSV, and SARS-CoV-2, the virus that causes Covid.
Researchers at Saarland University Hospital in Germany tested the spray on 450 adults, mainly in their early 30s. Participants were divided into two groups. One group received azelastine nasal spray, one puff in each nostril three times a day. The other group used a placebo spray following the same schedule. Over nearly two months, participants conducted Covid rapid tests twice weekly. The study, published in JAMA Internal Medicine, found a Covid infection rate of 2.2% in the azelastine group, compared to 6.7% in the placebo group. The spray also appeared to reduce other symptomatic respiratory infections.
Researchers are not entirely sure why azelastine helps prevent infections. One theory suggests the spray binds to the virus in the nasal mucosa, the moist tissue lining the nose. This may block the virus from entering cells and inhibit a key enzyme it uses to replicate. Another possibility is that azelastine interferes with the ACE2 receptor, the entry point Covid uses to infect human cells.
Dr. Robert Bals, professor of internal medicine and pneumology at Saarland University, noted the spray could serve as a practical, over-the-counter preventive tool during high-risk periods or in crowded indoor settings. He emphasized that the trial’s participants were young and generally healthy, and that vaccines remain the primary defense against Covid. Larger studies are needed before azelastine can be widely recommended, especially for vulnerable populations.
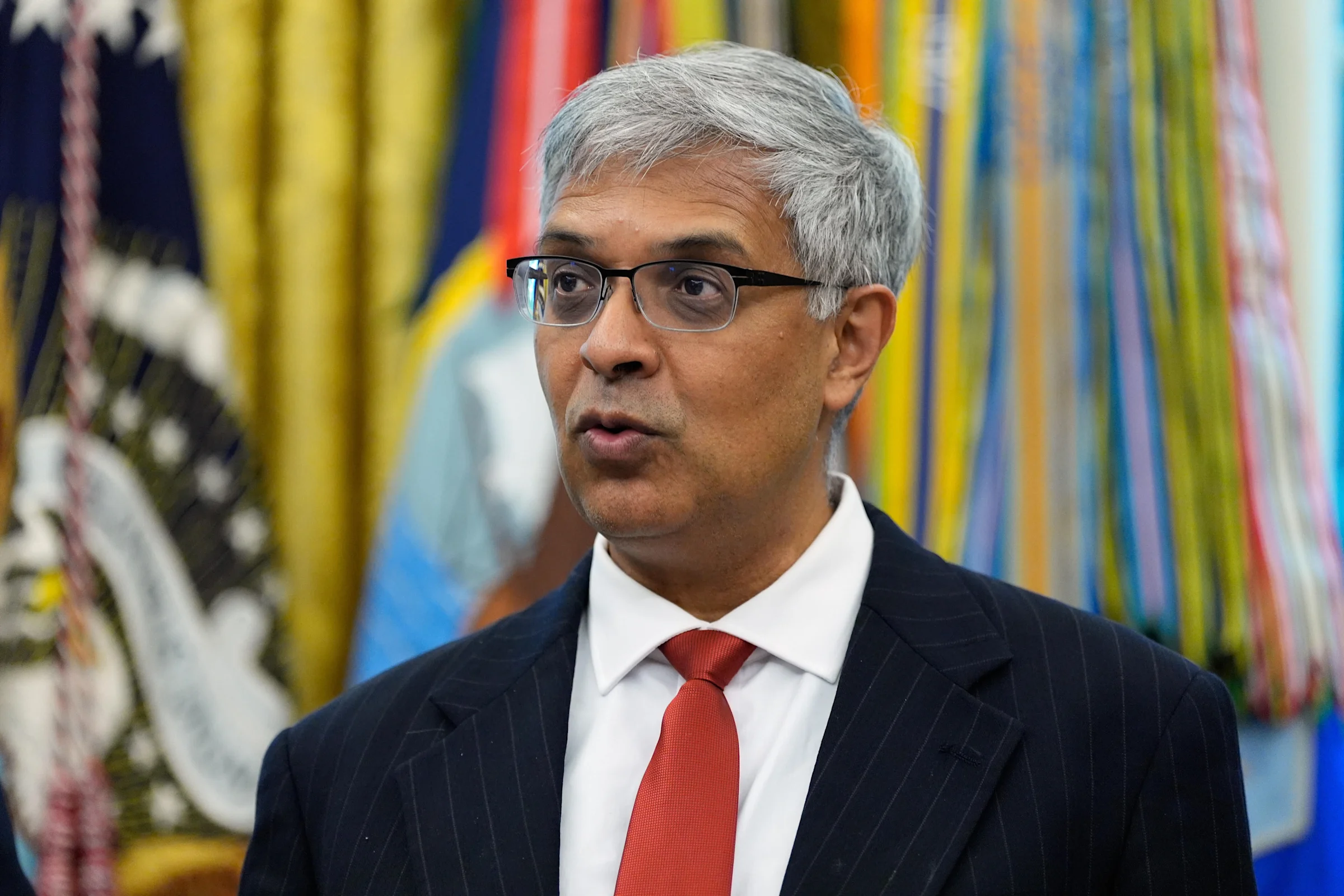
Independent experts have weighed in on the findings. Dr. William Messer, associate professor of molecular microbiology and immunology, described the results as promising but noted the challenge of maintaining a thrice-daily spray regimen. He suggested that masks might be easier to comply with for many people. Other researchers emphasized the need for data on older adults and immunocompromised individuals. Dr. Peter Chin-Hong, professor of infectious diseases, said azelastine could complement existing preventive measures for allergy sufferers. However, he cautioned that there is not enough evidence to recommend it widely as a Covid-blocking tool.
Despite these caveats, Chin-Hong highlighted the importance of the nasal mucosa as a target for future vaccines. He noted that current Covid vaccines do not fully prevent infection and called for more research on mucosal vaccines, similar to those used for influenza, as a strategy to block respiratory viruses more effectively.
The trial suggests azelastine nasal spray could offer a simple, accessible measure to reduce Covid risk. Its over-the-counter availability makes it scalable, and the antiviral properties observed against other respiratory infections are encouraging. Researchers caution that azelastine should not replace vaccination. Instead, it could serve as an additional preventive measure, particularly during periods of high transmission or in high-risk environments. Ongoing studies will be crucial to determine its effectiveness in older and immunocompromised populations and to explore the potential of nasal-based therapies and vaccines for broader respiratory virus prevention.